
REVIEW ARTICLE
AN OLDER WOMAN IN EARLY PREGNANCY: WHAT ANTENATAL SCREENING IS APPROPRIATE?
S Sulaiha Aznal MbChb(Glasgow), MG(Malaysia), International Medical University, Seremban
Address for correspondence: Dr Sharifah Sulaiha Syed Aznal, Senior Lecturer, Department of Obstetrics & Gynaecology, International Medical University, Clinical School, Seremban, Jalan Rasah, 70300, Negeri Sembilan, Malaysia. Tel: 06-7677798, Fax: 06-7677709, Email: shsulaiha_sydaznal@imu.edu.my
Aznal SS. An older woman in early pregnancy: what antenatal screening is appropriate? Malaysian Family Physician. 2008;3(3):xx-xx
Case scenario
A 40 years old Malay woman is amenorrhoeic for six weeks with no other symptoms of pregnancy. Urine pregnancy test is positive and transvaginal ultrasound confirmed a six-week intrauterine pregnancy. She had three previous uneventful pregnancies; her last childbirth was 7 years ago. She is concern about the risk of Down’s syndrome. She and her husband are against termination of pregnancy.
Questions
- What is the risk of chromosomal abnormalities in this pregnancy?
- How (and when) she should be screened for fetal abnormalities?
Answers
- When an older woman becomes pregnant, the issue of fetal abnormality is almost invariably a source of concern. This problem is likely to increase as more pregnancies are now occurring in women above 35 years of age. Although Down’s syndrome is the commonest chromosomal defect, other chromosomal defects are also more common as a woman ages, such as Edward syndrome (an extra chromosome 18) and Patau syndrome (an extra chromosome 13). Data from United States showed that the Down’s syndrome risk for a 25-year-old woman is about one in 1,250, rising gradually to one in 400 at 35 years (see Figure 1).1 For this woman who is 40 years old, her risk of getting a Down’s syndrome baby is about 1 in 100 (i.e. 1%).
Figure 1. Risk of Down’s syndrome baby by maternal age (adapted from Hook, et al1) - Since the early 70’s there have been various suggestions on the timing and combination of screening tests. They vary from first or second trimester or a combination of the two, together with serum markers and ultrasound (nuchal translucency and nasal bone) (see Figures 3 and 4). For many years, triple test performed in the second trimester (15th to 18th weeks of gestation) was the common test offered to women. It measures three serum markers: a-fetoprotein, β-human chorionic gonadotropin (hCG) and oestradiol where abnormal results will indicate higher risks for Down’s syndrome and neural tube defects. Recently, another marker called pregnancy-associated plasma protein A (PAPP-A) is found to be of use even earlier. Nevertheless, it has to be made clear that screening test is an indirect measure to indicate any pregnancy at high risk of fetal anomalies. It requires further confirmatory test if found abnormal; prenatal diagnostic tests such as chorionic villus sampling (CVS) or amniocentesis which are more invasive and of some risk of miscarriage.
Figure 2. Screening methods for Down’s syndrome
Screening using serum markers at first trimester seems to carry no larger advantage than if carried out at second trimester as the detection rate for Down’s syndrome is similar except that it allows a prenatal diagnostic test; chorionic villus sampling to be done after which a safer termination of pregnancy can be performed if so desired. However, Nicolaides2 who conducted a study on 44,613 pregnancies found that the detection rate certainly increased to 97% with false positive rate of 5% if the serum markers are incorporated with the evaluation of nasal bone and nuchal translucency. Malone et al has also concluded from his study that a combination of first trimester screening test (nuchal translucency and measurement of PAPP-A and free β-hCG) as early as 11 weeks gives sensitivity of 96% and specificity of 95% in detection rate.3
Table 1. Available methods of prenatal screening4,5
Screening methods |
Sensitivity |
Specificity |
| Maternal Age (MA) | 30 -50% | 85 -95% |
| MA + NT at 11-14 weeks | 70 -75% | 95 -98% |
| MA + NT + serum markers at 11-14 weeks | 80 -95% | 95 -98% |
| MA + NT + NB + serum markers at 11- 14 weeks | 90 -97% | 95 -98% |
| MA + serum markers at 15-18 weeks | 60 -70% | 95% |
MA - maternal age, NT- nuchal translucency, NB - nasal bone
Nuchal translucency and nasal bone tests via an early ultrasonography (best performed at 11 weeks) has been accepted as among the best ways to screen for fetal anomalies. The procedure requires a certain level of skill to performing it as the reliability of the test is operator and interpreter dependant. It requires an appropriate training to retain good views of fetuses at this gestation. The finding relies on the attitude of the fetus during measurement and accurate at specific angle (midsagittal plane obtained when the caliper is perpendicular to the nuchal fold). Time is also a factor as the fetal movement should be observed to differentiate between amnion and overlying fetal skin.
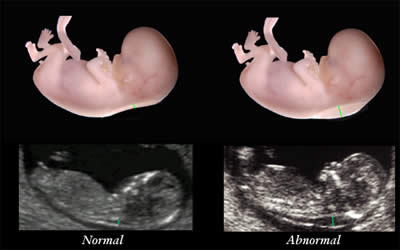
Figure 3. Nuchal translucency test measurements at 11 weeks of gestation
(Image reproduced with permission from Greggory DeVore, MD. http://www.fetal.com/NT%20Screening/02%20NT%20Imaging.html)
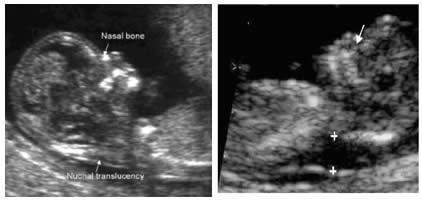
Figure 4. First trimester scan showing a normal nasal bone (left) and an absence nasal bone (right).
(Image reproduced with permission from KK Women’s and Children’s Hospital.
http://www.kkh.com.sg/PatientHealthLibrary/WomensHealth/First+Trimester+Screening/)
For most women in Malaysia, to be told that her pregnancy is normal and so as the fetus are the most reassuring matters during this physically and emotionally disturbing period. Nevertheless, there is still no one best approach. Issues involving cultural and religious differences have affected decision making of the women. Moreover, the law does not support the request for termination of pregnancy unless the abnormal fetus is lethal or carries potential harm to the mother.
However, the American College of Medical Genetics has come up with some recommendations as the following:7
- All women should have the option of invasive diagnostic testing for fetal aneuploidy by CVS, if available, or amniocentesis.
- For women who do not want any information regarding fetal aneuploidy status, following appropriate documentation, no other testing or screening is required.
- First trimester screening (NT, PAPP-A, and hCG) is an acceptable, cost effective approach for Down’s syndrome risk screening for women if they present early in pregnancy (before 14 weeks’ gestation).
- Incorporation of the nasal bone assessment into the first trimester screening protocol is optional and should be limited to clinicians who have specific training and participate in an ongoing quality assurance program.
- Women should be informed of the adjusted risk for Down’s syndrome and allowed to make decisions based on this number, because individuals will weigh risk/benefits differently and are capable of such decision-making. Because age is no longer used as a cutoff to offer invasive testing, it is no longer logical to use predetermined cutoffs based on age risk for screening programs.
- An NT measurement of 3.5 mm or greater, even in the setting of a low risk for aneuploidy screen result or normal fetal karyotype should prompt a detailed anatomic ultrasound, echocardiogram, or both.
- First trimester screening requires adherence to strict standards and maintenance of quality, both in the laboratory and ultrasound units. Sonographers must be appropriately trained in the proper technique of NT measurement and have appropriate certification through available organizations.
The majority of Malaysian pregnant mothers are first attended by primary care doctors whom may have basic knowledge and skill in obstetrics but less likely to have advanced training in feto-maternal medicine. There is a lack of awareness about the availability of screening tests and requirement for pre- and post-test counselling. The Ministry of Health has therefore recommended that antenatal screening tests for Down’s syndrome should not be performed routinely but made available to women who request to have it.8
Often, serum marker (triple test) is what commonly being offered in Malaysia though it is known that it gives little benefits in terms of time to perform. This cost roughly between RM150-200. Other markers are available on request. It is important that the gestation is confirmed and multiple pregnancies are excluded as it will affect the results. Prenatal diagnostic tests such as chorionic villus sampling or amniocentesis usually cost about RM800-1200. Ultrasound test for nuchal translucency and nasal bone however is inappropriate to be offered and conducted by health care providers who are not trained or qualified to do so thus proper referral to personnel who has the ability to do so is needed. It is also important that mothers who request to undergo the test should be thoroughly advised on the benefits and consequences of such procedure to her and the pregnancy.
Nevertheless, the current trend for early prenatal screening for Down’s syndrome in Malaysia is moving towards performing ultrasound measures looking at nuchal translucency and nasal bone as early as 11 weeks followed by proper genetic counselling and invasive diagnostic test if result is abnormal. Therefore for this woman, she should be offered such test with proper counselling on the consequences since she is still at very early of gestation.
References
- Hook EB, Cross PK, Schreinemachers DM. Chromosomal abnormality rates at amniocentesis and in live-born infants. JAMA.1983;249(15):2034-38 [PubMed]
- Nicolaides KH. Nuchal translucency and other first-trimester sonographic markers of chromosomal abnormalities. Am J Obstet Gynecol. 2004;191(1):45-67 [PubMed]
- Malone FD, Canick JA, Ball RH, et al. First-trimester or second-trimester screening, or both, for Down's syndrome. N Engl J Med. 2005;353(19):2001-11 [PubMed] [Full text]
- Saller DN Jr, Canick JA. Current methods of prenatal screening for Down syndrome and other fetal abnormalities. Clin Obstet Gynecol. 2008; 51(1):24-36 [PubMed]
- Simpson JL. Choosing the best prenatal screening protocol. N Engl J Med. 2005;353(19):2068-70 [PubMed]
- Single-step maternal serum screening for trisomy 21 in the era of combined or integrated screening. Gynecol Obstet Invest. 2004;58(4):221-4 [PubMed]
- Driscoll DAM, Gross SJM, for the Professional Practice and Guidelines Committee. First trimester diagnosis and screening for fetal aneuploidy. Genet Med. 2008;10(1):73-5 [PubMed]
- Members of expert committee. Maternal Screening for Fetal Abnormality. Health Technology Assessment Report MOH/PAK/59.03(TR) [Full text]
